People experiencing mental ill-health often experience stigma and discrimination. Discrimination interferes with relationships and connections to family, friends, workplaces, community and culture, and negatively impacts on the recovery process for people experiencing poor mental health.
Introduction
People experiencing mental ill-health often experience stigma and discrimination. Discrimination interferes with relationships and connections to family, friends, workplaces, community and culture, and negatively impacts on the recovery process for people experiencing poor mental health.
A key element of reducing institutional and individual discrimination is to strengthen community understanding. Strengthening community understanding helps people to identify and better understand the early signs of mental distress. The understanding and ensuing conduct of health professionals is particularly important as the lived experience of people with mental illness is directly affected by the skill, attitudes and behaviours of the professionals with whom they interact.
Short-term initiatives aimed at improving community understanding and mental health literacy are part of the solution; however, increased understanding is not always associated with a reduction in discriminatory behaviour and stigmatising attitudes. Evidence suggests that broad, longer term, anti-discrimination and anti-stigma initiatives have more success in reducing the experience of discrimination by people living with poor mental health.
In October, Relationships Australia’s online survey sought further understanding of mental health stigma by posing a few questions to visitors to our website.
Previous research finds that…
- Three out of four people with a mental illness report that they have experienced stigma, with particular vulnerable groups facing higher risk.
- Almost 340,000 Australians have both mental illness and substance use problems. People with co-morbid problems are often discriminated against, judged and marginalised from services and the community.
- Same-sex attraction, gender dysphoria and intersex conditions make people more vulnerable to discrimination and this leads to a higher prevalence of mental ill health for these people. In one Australian study, 38% of same-sex attracted female respondents had experienced depression compared to 19% of heterosexual female respondents, and non-heterosexual women were almost four times more likely to have tried to harm or kill themselves.
- Research confirms that it is almost impossible to separate the existence of a mental health condition from the experience of racial discrimination, and as such, discussions of mental health stigmatisation, in particular, faced by Aboriginal and Torres Strait Islander people with poor mental health need to acknowledge their lived experience of racial discrimination.
Survey Results Analysis
More than 2600 people responded to the Relationships Australia online survey in October. Around four‑fifths of survey respondents (81%) identified as female.
As was the case for last month’s survey, more females than males responded in every age group (figure 1). More than eighty-five per cent of survey respondents were aged between 20‑59 years, with the highest number of responses collected for women aged between 30-39 years (inclusive).
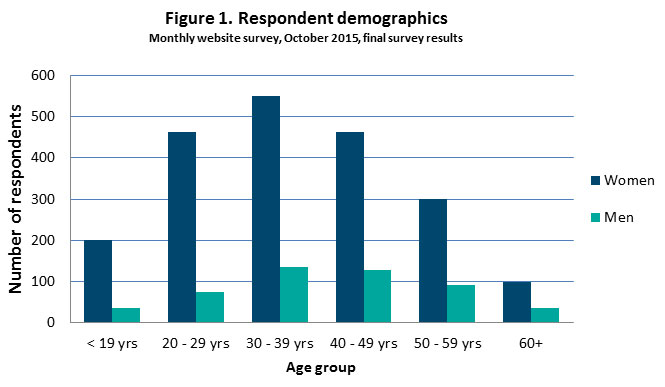
The demographic profile of survey respondents remains consistent with our experience of the people that would be accessing the Relationships Australia website.
More than fifty per cent of survey respondents indicated that they were married or living with someone in a relationship. One-sixth indicated that had never married and a further one-sixth of survey respondents were separated or divorced.
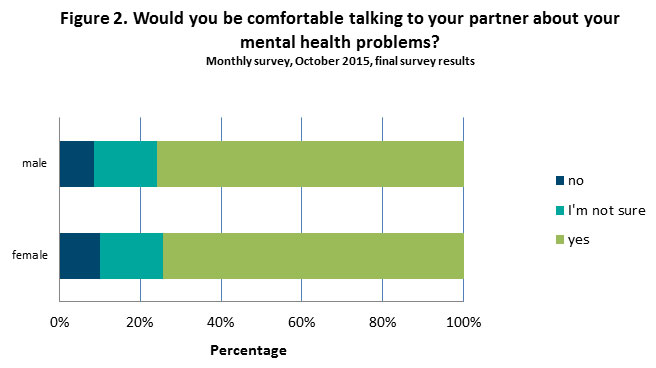
Three-quarters of men and women survey respondents reported that they would be comfortable talking to their partner about mental health problems (figure 2). Around one-sixth (16%) were not sure whether they would be comfortable, and a further ten per cent indicated they would not be comfortable.
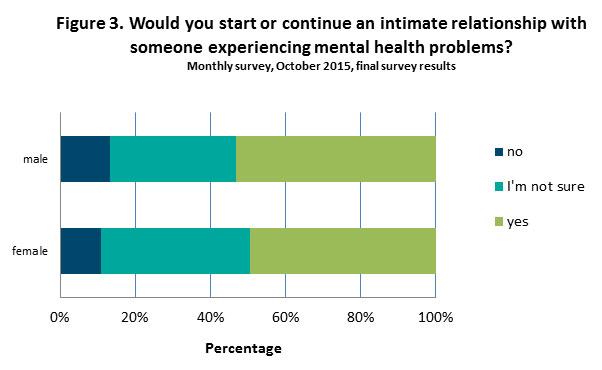
People were less certain when asked whether they would start or continue an intimate relationship with someone experiencing mental health problems. Fifty per cent of survey respondents indicated they would start or continue an intimate relationship with someone experiencing mental health problems; however, almost forty per cent (38%) indicated they were unsure. A further 11 per cent indicated they would not start or continue an intimate relationship with someone experiencing mental health problems (figure 3).
Not surprisingly, men and women who were married or living in a relationship with someone were more likely to report that they would be comfortable talking to their partner about their mental health problems that people who reported they were single or divorced/separated.
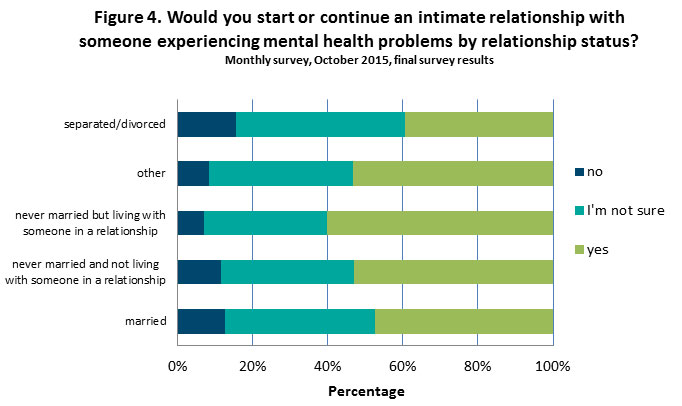
Men and women who were separated/divorced (53%) or married (61%) were the least likely to indicate that they would start or continue an intimate relationship with someone experiencing mental health problems (figure 4). In contrast, just under two-thirds (60%) of survey respondents who indicated they had never married but were living with someone in a relationship were the most likely to report they would start or continue an intimate relationship with someone experiencing mental health problems.
References
National Mental Health Commission. A Contributing Life, the 2012 National Report Card on Mental Health and Suicide Prevention. Sydney, NMHC, 2012.
Reavley, N.J. and Jorm A.F. (2011) Stigmatizing attitudes towards people with mental disorders: findings from an Australian National Survey of Mental Health Literacy and Stigma. Aust N Z J Psychiatry. Dec. 45(12):1086-93.
Sacks, S., Chaple, M., Sirikantraporn, J., Sacks, J.Y., Knickman, J., Martinez, J. (2013) Improving the capability to provide integrated mental health and substance abuse services in a state system of outpatient care. Journal of Substance Abuse and Treatment, 44(5): 488-93.
